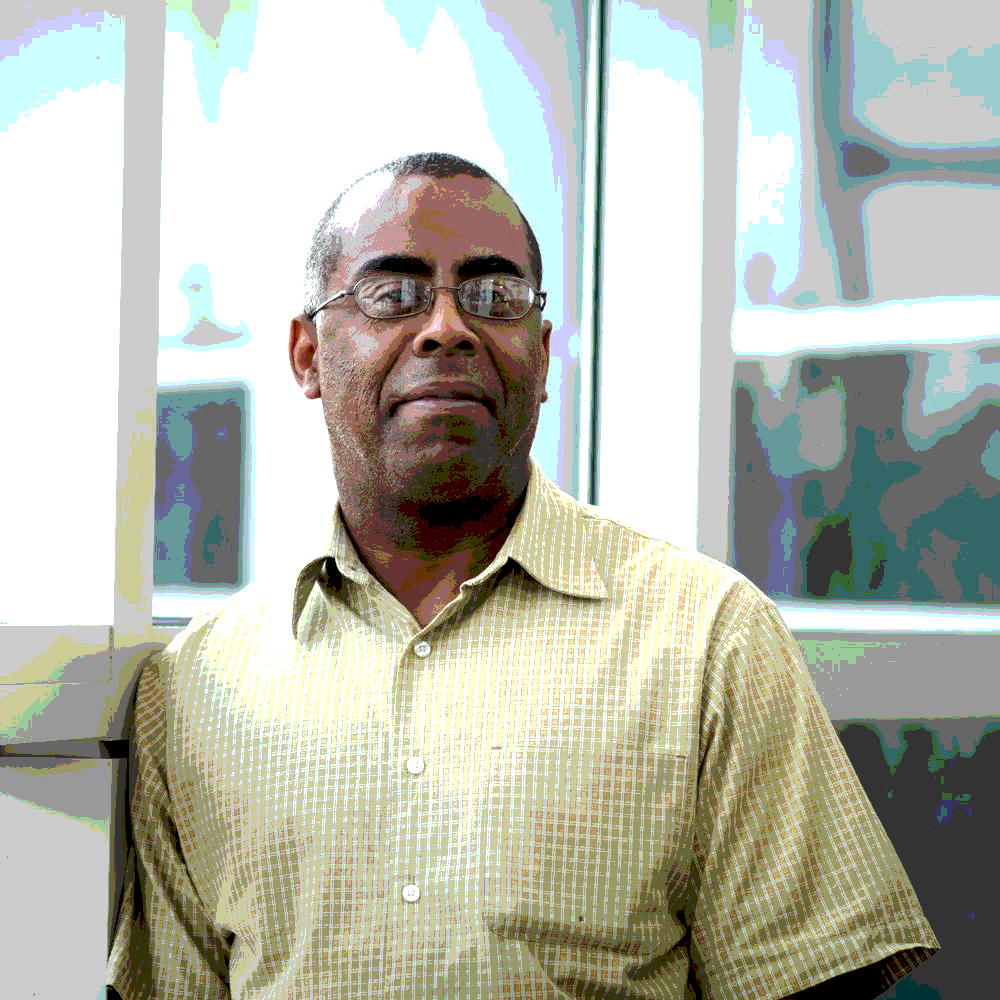
Chris Wade
HIV Project Coordinator / Prevention Lead Agent
Illinois Public Health Association
Interviewed in July 2020
Q: Could you define HIV stigma in your own words?
A: “To me, HIV stigma is many layers of negative attitudes, mindsets, and feelings about people living with HIV, as well as about folks that care for and have compassion for people living with HIV. It’s almost like you’re a pariah because you managed to contract a disease that people have made – well, 1) that has been (unjustly) criminalized and 2) people think that you chose to take this risk. And unfortunately, some of us, maybe didn’t know and maybe our partners didn’t know at the time. So it just really kind of speaks volumes. It’s similar to racism: it’s the labeling of individuals, simply because of a disease that they have. That because you’re gay, you’re going to have HIV.”
Q: You mentioned stigma coming at people who care for people with HIV. Can you explore that a little bit more?
A: “Yeah. People can go after caretakers, as well as people who might be married to, engaged to, or in relationship with a person living with HIV. It’s this idea of “why would you do that? Aren’t you afraid of becoming HIV positive?” And that goes into the lack of education and ignorance that folks have out there in the community about these advances in medical treatment. Basically, HIV is a chronic disease that folks can live with and still lead happy, normal lives. But unlike most chronic diseases (i.e. diabetes, cancer) you have the stigma that comes with HIV/AIDS. I feel like I’m living through three epidemics: COVID, racism and HIV. When you look at all this, you can see that we’re finding ourselves in the same position, dealing with the same population.”
Q: Why do you think stigma exists?
A: “Given our current time that we’re in – with relation to the Black Lives Matter movement and racism – it’s a feeling of supremacy. Being better than them. Greater than. And we live in a world today where people feel like they’re better off if they can look down on a group.”
Q: What do you think the root causes of stigma are?
A:”I think it can be environmental, it can be your social network and your circles, and it can be cultural. I’ll say that particularly with the black and brown communities, (living with HIV) is still taboo. It’s still something that, unfortunately, the community has not embraced. Whatever beliefs (about HIV) individuals have, I think they are deep-rooted within the HIV community as the stigma permeates these groups. There’s clear indications of the social determinants of health within certain populations, and we need to start addressing that.”
Q: Has HIV stigma ever had a negative impact on your life, and how so?
A: “Yeah, on so many levels as I reflect back. I’ve had to come to terms with the fact that I’m not living with HIV, HIV lives with me, and I’ve had to overcome this. When I first got diagnosed, that was the hardest two years of my life. I was told that I wouldn’t be around in six years, and as a person of color, I knew that was probably factual. I tested positive in 1992, so I’ve been living with this virus for about 28, 29 years now. And what’s supposed to happen? A lot of my friends – drug users, sex workers – dead. All of them. Some of the negative impact it has had on my life – particularly with having been in sex work, and engaging in activities – is the fear of, well, what if someone makes an allegation that I did not disclose? Or what if I get jacked up by the police, and they test me? I’ve been hanging out on the corner, getting picked up, and they know this and want to throw a charge at me. Other aspects of it were within my family. It’s folks not understanding my lifestyle as a same-gender-loving male living with HIV. You have folks that still are under a belief that gay men are pedophiles that will go after your kid. So yeah, it’s hit me particularly in the ways that I’ve mentioned. And thank God I’ve been in positions and environments with people who are advocating against a lot of that, trying to change a lot of the rules and policies and laws as relates to some of this, and educating folks. I can educate by talking to other black men or women with relation to living my life as HIV positive.”
Q: Yeah, we’ve certainly come a long way since the 1980s, but then to kind of have these reversals where people try to turn back the clock must be really frustrating.
A: “It’s funny you say that, because I feel like I’m living through three epidemics: COVID, racism and HIV. When you look at all this, you can see that we’re finding ourselves in the same position, dealing with the same population. And it’s like, we’ve had 400 years of racism, we had almost 40 years of HIV, and we’re going into how many months with COVID now. So, there’s clear indications of the social determinants of health within certain populations, and we need to start addressing that. I think it all starts with booting out racism, and people becoming anti-racist moving forward. It has to be intentional, and it has to be led by groups of color because often you have these entities, groups or bodies who think they know what’s in the best interest of certain populations without asking those populations. Stigma intersects with so many pieces of our lives that it can be detrimental to our health because, since you’re probably less likely to seek help, you’re probably less likely to talk about it.”
Q: Has HIV stigma ever made you hesitant to receive HIV testing or treatment, and how so?
A: “Yes. I would say that the way stigma is, it does deter people from getting tested, but at that time, it was the thing to do. We normalized it. As homeless, drug using, sex-working people, we normalized it amongst ourselves. Some of it was that you knew you might get off the streets because now you’re going to get taken care of: you’re going to qualify for Social Security disability, you’re going to get housing, medical care, food, and all these necessities that you didn’t have. So that was incentive and motivation to go get tested. Now, let’s talk about the environment of HIV care and being HIV positive. Unfortunately, there’s stigma within those environments. There’s the stigma around coming in and healthcare professionals thinking “Oh, you’ve got an STD. That means you’re having unprotected sex.” And now you’re scared. Are they going to turn me in? Are they going to report me to the state? Am I going to be made to feel less than? Do I even bother to share and get treated? Do I go somewhere else where they won’t know my status?”
Q: What do you think needs to be done to overcome HIV stigma?
A: “There has to be campaigns, like what we’re doing here with Illinois HIV Care Connect. They have to be put front and center and done intentionally with marketing and media that puts HIV front and center and puts the population’s most impacted front and center. What we’ve been trying to do here at Illinois HIV Care Connect with our social media marketing campaigns is actually giving money to agencies with CDC content so that they can put billboards up, bus signs up, etc., of what the virus currently looks like today, which is (predominately affecting) black and brown men. Making sure that these young men feel like they’re being seen. HIV and AIDS activists changed the landscape of healthcare. Had it not been for a lot of HIV activists, a lot of the medications that come out of the FDA would have dragged on, dragged on, and dragged on.”
Q: How would overcoming stigma benefit a person living with HIV?
A: “I think it would benefit their health outcomes. Stigma intersects with so many pieces of our lives that it can be detrimental to our health because, since you’re probably less likely to seek help, you’re probably less likely to talk about it. And it will consume. It really will consume you. And it will lead to the worst possible health outcomes for an individual. I think that us doing our part as a community and as far as healthcare providers, we’ve got to treat this like any other disease and stop making people feel less than. Most people feel the only way you’re going to get HIV is through sex or IV drug use. People forget that we also have a huge population of young people that were born with this virus, and that population is struggling in so many senses because they’ve been in pediatric care and now, they’re switching into adult care. Unfortunately, I think we have providers and folks in the community that just don’t get it when it comes to that population because that’s a whole other dynamic. They didn’t have a choice. They had no choice in living with this virus.”
Q: Are there community resources or educational materials that you have found helpful?
A: “Yeah. I definitely think that folks should check out the Illinois HIV Care Connect program. I think that folks should surf the net and look at information coming out of the CDC, their state departments of public health, their local departments of public health, and programs that are by, for and about people living with HIV. I have found those to be the most helpful. HIV and AIDS activists changed the landscape of healthcare. Had it not been for a lot of HIV activists, a lot of the medications that come out of the FDA would have dragged on, dragged on, and dragged on. That process was expedited because of activists, and it benefited not just people living with HIV, but other people with chronic illness. So it’s interesting to not only find out and learn that history, but to be a part of that history and continue to activate and advocate in your communities to get things done. I mean, we still have a long way to go unfortunately. There will be people talking about U=U, undetectable equals untransmittable. We have to be careful with that messaging because I have friends, personal friends, that I know will never be able to achieve viral suppression (because their bodies have developed a resistance to HIV medications). So how would I make them feel if all the messaging I keep putting out said, “U=U, everybody get to viral suppression.” How do we make those folks that are now left out of the conversation feel?”