Pre-exposure prophylaxis (PrEP) for HIV-negative individuals at high risk for HIV infection
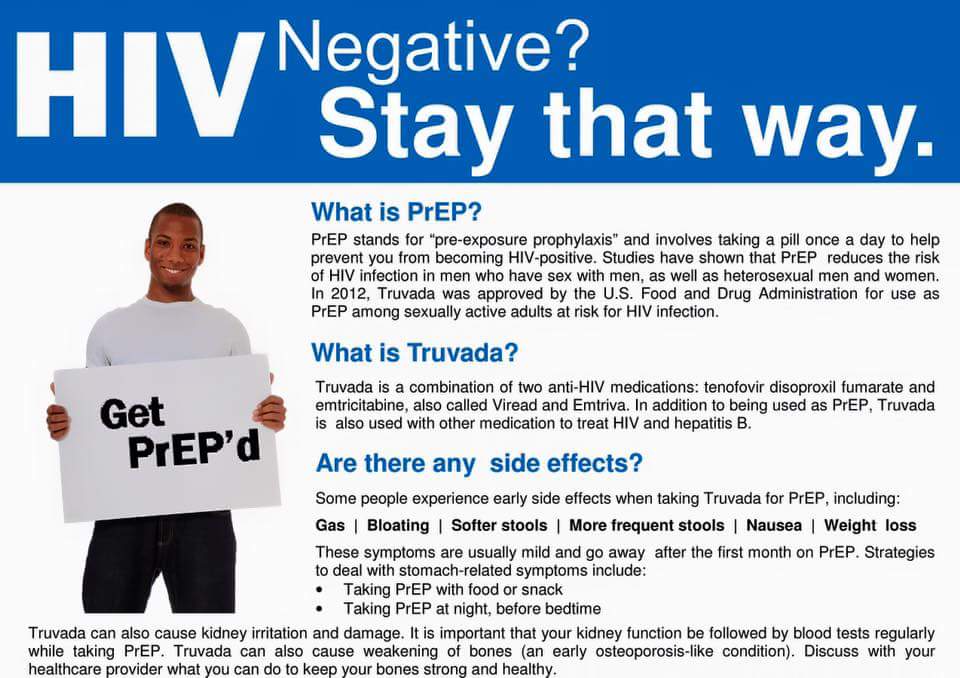
While treatment as prevention (TasP) involves prescribing antitretroviral treatment (ART) to HIV-positive individuals to lessen the risk of them passing the HIV infection onto others, PrEP is a prevention strategy that involves providing ART to HIV-negative individuals to protect them from contracting HIV. While TasP may be recommended along with condom use to a monogamous couple in which one individual is HIV-positive and the other HIV-negative, PrEP may be recommended for individuals at high risk for HIV infection, such as men who have had anal sex without a condom, individuals with multiple sex partners or a history of sexually transmitted infections (STIs), sex workers and injectable drug users. By consistently taking ART before any possible HIV exposure occurs, an individual can reduce the risk of HIV infection by up to 92 percent, according to the Centers for Disease Control and Prevention (CDC).
According to CDC recommendations, providers should assess a patient’s HIV risk factors and provide an HIV test before prescribing and renewing PrEP. Tests for STIs, kidney function and hepatitis B are recommended, as well as extensive and ongoing counseling on risk-reduction, adherence and condom use.
Prevention of mother-to-child transmission (PMTCT)
Since the mid-1990s, ART has been used to decrease mother-to-child transmission of HIV. In Illinois, ART medications have decreased newborn HIV infection by 99 percent. AZT (zidovudine, Retrovir) can be given to pregnant HIV-positive women to prevent transmitting HIV to their children, according to Aidsinfo.nih.gov. In addition, single-dose nevirapine can be given during labor and to the newborn, according to the National Institute of Child Health and Human Development. For six weeks after birth, babies are also given AZT. HIV blood testing for babies born to HIV-positive mothers is recommended at 14 to 21 days after birth, at one to two months, and again at four to six months. If the results on two of these blood tests are negative, the baby is not infected with HIV, according to Aidsinfo.nih.gov.
Post-exposure prophylaxis (PEP) for single-event exposure to HIV
PEP has been used since 1998 as a short-term treatment for those who have already been exposed to HIV. Those exposed during a single event – such as a sexually assaulted person, an individual having unprotected sex with an HIV-positive or status unknown individual, a health care worker exposed to HIV-infected fluids, or a drug user sharing a needle – have been offered PEP as an HIV treatment strategy. The use of AZT was popular in PEP, but AZT has recently been replaced by a three-drug treatment combination of tenofovir, emtricitabine and raltegravir, according to HIV clinical guidelines. To be most effective, PEP should be started immediately after exposure.